Healthcare 2022: “Follow the _______”
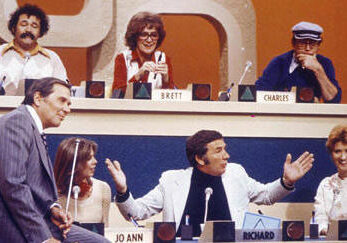
One of my favorite game shows from childhood, Match Game, has been rebooted in the last few years. Near the end, a contestant tries to guess the most popular answer to a question or phrase. They ask 3 opinions from the celebrity panel for advice, and ultimately present their own best guess; sometimes to applause, sometimes to boos and groans. Often the answer seems so obvious to us watching at home, that we find ourselves yelling at the contestant through our screens, “How did you miss that?”
As an executive turned caregiver turned patient turned executive again, I’ve touched pretty much every point in the healthcare ecosystem in the work I’ve done or the diagnoses I’ve endured. On a global scale, we’ve been on quite a healthcare journey here, and it’s tough to predict where we’re going. We’re all looking for someone or something to lead the way. I’ll offer a few ideas from my own lived experience, and as Gene Rayburn said back in my day, “You may choose one of these, or give us one of your own.”
- Follow the Physician (Inclusive of Clinician)
I’ve followed quite a few physicians; whether it was down the hall for a diagnosis code or documentation to code a visit properly and get them paid, for a signature for drug samples as a pharmaceutical rep, or for advice on how to beat cancer. I’ve had the great fortune to work with some brilliant and compassionate physicians. But one thing we know: they are burned out. We know the costs of physician burnout to the U.S. healthcare industry are $4.6 billion per year, mostly due to turnover and reduced clinical hours. That’s an annual cost of $7,600 per employed physician per year. And we know that the problem of burnout has been here for a while. According to the Medscape National Physician Burnout & Suicide Report 2021, 79% of physicians stated that their burnout had started before the COVID-19 pandemic. That’s only gotten worse now. I’m guessing physicians aren’t looking for any additional responsibility than they already have, not to mention the insidious “alert fatigue” and other digital health boons yet burdens. Let’s give our frontline healthcare workers a collective hug and leave them off the answer board for now while they recover from a job that they didn’t sign on for.
- Follow the Payor
My internship in graduate school for an insurance company wasn’t one of my more favorite stops along my mosaic career. I didn’t feel great about attaching a dollar value to a “covered life” or saying “per member per month” more than my own name. Assessing risk of health status is important, but I believe we still have it all wrong in terms of incentivizing “being healthy” vs. “being sick.” We’re still not seeing the behavior change we need to decrease overall spending. Until I see all employers giving PTO for colonoscopies and mammograms, I will continue think that healthcare benefits are broken. And until I don’t have to fight for equipment and nursing services for my permanently disabled son or scans for cancer patients, I will continue to think that insurance companies are not seeing the bigger picture of the consumer they serve. This answer doesn’t make the board either.
- Follow the Policy
“Big goals require big efforts,” says Abner Mason, founder and CEO of ConsejoSano, meaning if we want to help create a healthier, more equitable world, it’s going to have to come from rules and regulations set forth by lawmakers on a local, state, and national level. As we optimistically look forward to how the recently passed Infrastructure Investment and Jobs Act (IIJA) will improve broadband availability for millions of Americans, we anxiously await permanent rulings on telehealth post-pandemic. I celebrated the impact of advocacy after stumping on Capitol Hill for Fight Colorectal Cancer. We were able to eliminate the Medicare loophole for screening colonoscopies. And we’ve seen the impact of the Final Rule of the Cures Act to give patients and their healthcare providers secure access to health information and greater interoperability. There is power in policy. Therefore, I’m awarding the $2000 answer to policy because I feel it holds the greatest potential for the greatest number of people.
- Follow the Patient (Inclusive of Caregiver)
To those who follow me, you’re expecting this to be my preferred answer, and you’re correct, with certain caveats. When I read a report from StartUp Health showing that the greatest VC investment is in Patient Empowerment Tools but the least is in Education and Content, I know that we are not doing enough to close the health and digital literacy divide. How can we follow the patient when we’re not empowering or engaging us to take an active role in our care (I identify as a patient since I have a chronic health condition)? It’s setting us up for failure. It’s time for patients to take a legitimate seat at the table because as my friend and colleague Gil Bashe routinely says, “It’s their table.” How do we train patients to be “franchise players”, not only for our own health, but also to add value to the business of healthcare (biotech, health systems, pharma, IT) as a whole? Jessica Scott et al collaborated on an excellent guide that when implemented with the help of patient experts should be a gamechanger in the way patients become stakeholders in rightsizing our health future. $3000 answer here.
But what is the $5000 answer? If we can agree that 2020 was the problem, and 2021 was the proclamation of the problem, then sticking with the “P” alliteration, my winner would be “Follow the Process.” In short, we’ve done a lot of talking about what’s wrong – 2022 should be the year we start doing. The process is a collaboration of representatives from each of the four above stakeholder groups on a level playing field with a bonus answer of “Follow the Data” (right, John Nosta!?!). Instead of throwing up our hands and accepting the status quo of “we can’t do that because,” let’s instead ask questions and create paths forward for “now we can!”
“How did you miss that?” (TIC)